Wisdom teeth are those pesky third set of molars that usually appear between the ages of 17 and 25. These teeth are prone to infection due to their position at the back of the mouth and the difficulty of keeping them clean. In those cases, a wisdom teeth infection can progress quickly from minor discomfort to a serious health issue if left untreated, so early detection and treatment are crucial.
Wisdom tooth infections can affect not only the wisdom tooth itself but also surrounding teeth and gums, impacting overall oral health. That’s why it’s crucial to avoid wisdom teeth infections and catch them early so you can seek treatment from a dental professional.

What Triggers Wisdom Tooth Infections
The main cause of wisdom tooth infections is bacterial buildup around impacted or partially erupted wisdom teeth. When teeth can’t come in properly, they create pockets where bacteria thrive, leading to inflammation.
Pericoronitis, the inflammation of the gum tissue around your wisdom teeth, occurs when food particles and plaque get trapped under the gum flaps covering erupting wisdom teeth. Poor oral hygiene makes things worse. This is because the position of wisdom teeth makes them very difficult to clean properly, and bacteria can establish themselves even with good hygiene habits.
Other risk factors for wisdom teeth infection include gum disease, crowded jaws that prevent proper eruption, smoking, high-sugar diets, and a compromised immune system.

Gum Disease and Wisdom Teeth Infection
When bacteria accumulate in the gum tissue around a wisdom tooth, especially one that is partially erupted or impacted, it can lead to inflammation and infection. This can result in swollen gums, bad breath, and difficulty chewing due to discomfort in the affected area.
At the same time, if gum disease is present, it can exacerbate and complicate wisdom tooth infections, making them more severe and harder to treat. This creates a vicious cycle that allows harmful bacteria to thrive, thereby increasing the risk of other oral health problems.

Recognising Infected Wisdom Tooth Symptoms
Infected wisdom tooth symptoms start as localised discomfort but can escalate fast. Early-stage wisdom tooth infections may manifest as persistent throbbing pain around the affected tooth, which can radiate to the ear, jaw or neck. Jaw pain is common, mainly when the infection spreads or the tooth is impacted. This infected wisdom tooth pain worsens when chewing or opening the mouth wide.
Other ways for how to know if a wisdom tooth is infected include red, swollen gums around the wisdom tooth, often accompanied by a foul taste or odour. Gum pain is another common symptom. Importantly, pus discharge indicates an active bacterial infection that needs immediate attention. Bleeding when brushing or eating may also be a common occurrence.
Systemic symptoms develop as the infection spreads, including fever, swollen lymph nodes and fatigue, which indicate that the body is fighting a serious infection. Difficulty opening the mouth fully –trismus, constriction of the jaw – can also occur, which may affect your ability to eat and speak.
Normal eruption causes mild pressure and occasional discomfort, but infected wisdom tooth symptoms progress to persistent pain, visible inflammation, discharge and worsening symptoms over time.

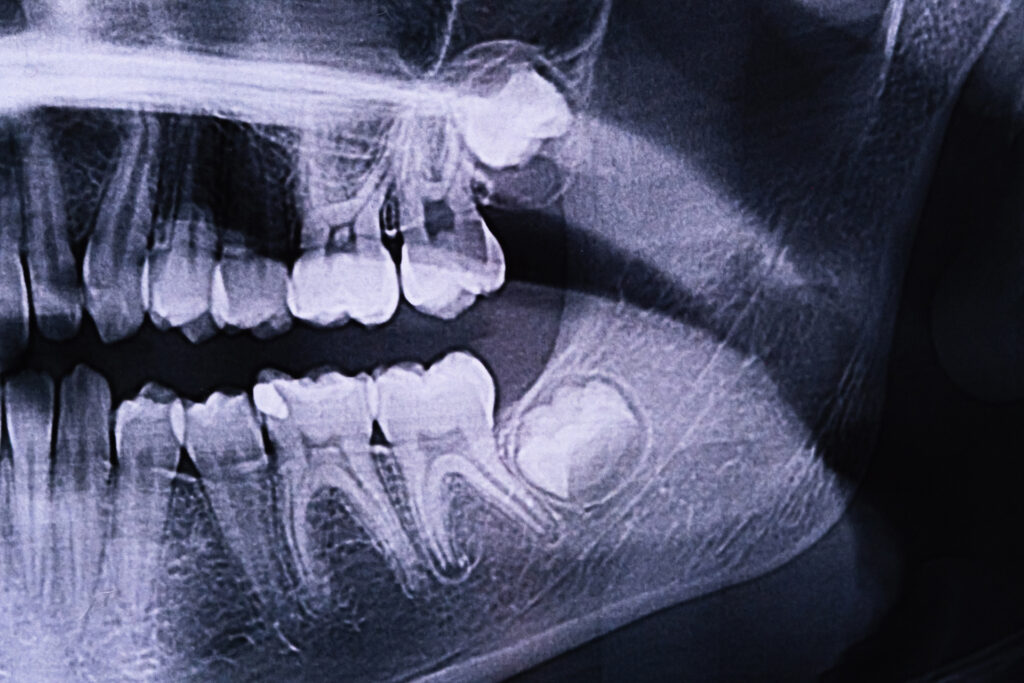
Connection Between Impaction and Infection
Impacted wisdom teeth are a strong predictor of infection problems. Impaction occurs when there is not enough jaw space for the tooth to emerge fully, causing partial or full entrapment under the gum line.
Different impaction types have their own infection risks. Partial impaction creates bacteria-trapping pockets, making a partially impacted wisdom tooth more prone to infection. Complete impaction can lead to the formation of a cyst. Angular impaction damages adjacent teeth and creates hard-to-clean spaces. Horizontal impaction, where teeth lie sideways and press against the second molars, is the most problematic.
Dental X-rays and panoramic imaging can identify impaction patterns early, allowing for preventive treatment before symptoms develop.

Consequences of Untreated Infections
Wisdom tooth infections rarely stay localised. If a wisdom tooth infection is ignored, it can lead to serious oral and systemic health risks. Infection spreads to adjacent teeth, causing decay and gum disease in otherwise healthy areas. The proximity to vital structures means that infection can spread to deeper tissues, including the jawbone.
Abscess formation creates pockets of pus, causing severe pain and swelling. Effects also extend beyond oral health, can impact sinus cavities and cause chronic fatigue, eating difficulties and bad breath. Long-term consequences include damage to adjacent teeth, bone loss and cyst development, which may require extensive treatment. In extreme cases, bacteria can enter the bloodstream and cause life-threatening systemic infections. If not managed properly, a wisdom tooth infection can lead to future problems and additional infections. Timely dental intervention is crucial.

Professional Diagnosis and Assessment
Dentists use multiple approaches to diagnose wisdom tooth infections. Clinical examination includes visual inspection, assessment of swelling and gentle palpation to identify tender areas and abscesses.
Advanced imaging provides crucial information about the extent of the infection and the tooth’s positioning. Digital X-rays show bone loss and decay patterns. Panoramic radiographs provide a comprehensive view of all wisdom teeth, helping to identify current problems and predict future complications. Imaging also helps assess the condition of nearby teeth that may be affected by wisdom tooth infection.
Treatment Approaches for Wisdom Tooth Infection
Initial wisdom tooth infection treatment focuses on controlling infection and managing symptoms. Antibiotics target bacterial infections, and antiseptic rinses reduce the bacterial load in the mouth. Pain management may include prescription medications and anti-inflammatory drugs like ibuprofen or acetaminophen to alleviate discomfort.
However, medication alone rarely provides a permanent solution. The most important way on how to treat wisdom teeth infections is to extract the offending wisdom tooth. Wisdom tooth extraction, also known as wisdom tooth removal, is often recommended to prevent infections and address the underlying issue. Local anaesthesia is used during the procedure to ensure patient comfort. Surgical complexity varies depending on the tooth’s position. Some methods can be performed in a general dental office, while others require a referral to an oral surgeon.
Recovery from wisdom teeth infections takes several days of rest and careful post-operative care. Most patients feel significant relief within the first week. For many people, having wisdom teeth removed can help prevent future infections and complications associated with these teeth.

Prevention Strategies and Early Intervention
Preventing wisdom tooth infections requires specialised cleaning techniques, including longer-handled toothbrushes, interdental brushes, and water flossers that can reach the back areas of the mouth more effectively.
Dietary habits also play an important role. Reducing sugar limits bacterial growth, and staying hydrated helps maintain healthy saliva flow, which in turn supports natural mouth cleansing. Quitting smoking also improves wound healing and reduces the risk of infection for wisdom teeth.
Perhaps one of the most vital strategies is to attend regular dental check-ups, as these allow your dentist to detect problems early before painful infections in wisdom teeth can develop.

Special Considerations for Young Patients
Teenagers and young adults are at the highest risk of wisdom tooth infections due to the timing of their eruption and lifestyle factors. This age group often has irregular dental care, high sugar consumption, and may delay treatment due to costs or dental anxiety.
Early monitoring during adolescence enables the identification of problems before symptoms emerge. Younger patients typically heal faster from extractions, but treatment planning must also consider their ongoing orthodontic needs.

Home Management
While professional treatment is essential, certain home remedies can provide temporary relief from wisdom teeth infections. Warm saltwater rinses reduce the bacterial load and soothe inflamed tissues. Cold compresses minimise swelling and provide infected wisdom tooth pain relief. Over-the-counter pain relievers offer temporary symptom management, which can be helpful if you have to wait some time before your dental appointment. However, patients must understand that delaying professional care allows infections to spread and become more serious.
There are also critical warning signs that demand immediate attention. These include persistent fever, difficulty swallowing or breathing, severe facial swelling and unresponsive pain. If these symptoms arise, this may signal a spreading infection that requires urgent dental attention.

Timely Professional Care is Key
Knowing how to recognise a wisdom tooth infection and seeking professional help promptly can prevent minor issues from developing into more significant health problems. Early-stage wisdom tooth infections respond better to conservative treatment than advanced infections, which may require major surgery.
The key to successful wisdom tooth infection treatment is to spot the symptoms early and work with experienced dental professionals who can assess and plan the treatment. In all cases, regular monitoring and preventive care are the best protection against complications.
For patients experiencing wisdom tooth pain or a suspected infection, seeking professional help is the best way to achieve relief and maintain long-term oral health. The team at TEETH @ Tiong Bahru offers wisdom tooth evaluation and treatment options for every patient. Book an appointment with us today to start your journey to resolving your wisdom tooth infection.
RELATED WISDOM TOOTH EXTRACTIONS